Some time back, I wrote about the importance of clearing the roof of debris. Like many things I write, it was intended as a metaphor, illustrated by happenstance with imagery of me clearing actual debris off my actual roof. Because sometimes, in spite of life’s special curve balls, we have to muster the energy and resolve to do stuff that simply needs to be done. And in so doing, perhaps we can find joy or a sense of gratification, and maybe even extend that process to a more metaphysical level, using it as a tool for release or letting go, or at the very least, we can check one more thing off the ever-growing list and move along to the next item.
Which, in this case, is a roof sealant.
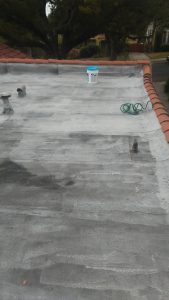
Last winter, we enjoyed the heaviest amount of rainfall that Los Angeles has seen in years. Although not enough to entirely counter the trend of drought that has plagued the region, it did refill reservoirs and contribute to record snowpack in the mountains, dramatically relieving the strain on water reserves. However, this exceptional amount of rain also managed to seep through the apparent (but not obvious) cracks in our roof, puckering the paint in our kitchen ceiling. While the roof remains structurally sound, the asphalt sheeting is showing its age and beginning to crack under the incessant heat of the sun.
When a minor leak from our water heater led to a small amount of construction in our kitchen, we ended up repainting the entire room and fixing the ceiling in the process. Of course, that will look fabulous up until the time when we have another multi-day deluge. Continue reading Sealing the Roof