Dear Readers
It’s with a heavy heart that I write this message. My younger brother Jeffrey Poehlmann passed away from complications due to a sudden and fierce reoccurrence of his lung cancer in his “good” lung. Jeff, as you all know from reading this blog, spent the last four years of his life with the knowledge that he had an unwelcome and invasive guest in his body and forged ahead every day looking to the future and taking as much positive living in the moments as he could. He knew he was working on borrowed time and wanted to do as much good as he could for the advancement of lung cancer awareness through this blog, his writing for www.lungcancer.net, and his Patreon site. Hopefully, we will be able to round up all this writing in book form at some point, one of the goals he had in mind from the start.
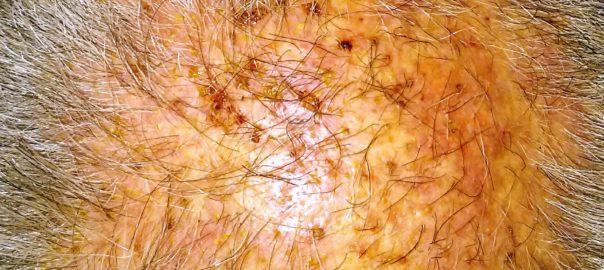
Jeffrey’s last treatment, which you read about, was taking its toll. The Poziotiniv chemo treatment began May 23rd. This targeted therapy was appearing to work incredibly well at reducing the main tumor marker and other metastases, while at the same time providing a litany of other symptoms including a full body rash that all his remaining energies went to battling. Since the 26th of September, Jeffrey’s doctors took him off these meds to give his body a chance to recover.
He subsequently developed what appeared to everyone to be pneumonia. As pneumonia symptoms seemed to progress and his cough kept him from any sleep, Jeff began taking oxygen on October 10th during his last week at home. On Thursday morning, while his wife was at work and daughter at school, Jeff called an Uber to take him over to USC Norris Comprehensive Cancer Center for evaluations.
That Thursday the x-rays showed complications in his formerly good lung; he was placed in a private room in ICU. His lung was then drained giving Jeff incredible relief and the ability to feel well enough to easily communicate and had what he called his most restful and full sleep in weeks that night. Unfortuntately, the bronchoscopy on Friday showed a huge cancer invasion of the lung and it was obvious to the hospital staff that he wasn’t long for this world.
With his typical good nature and positive outlook, Jeff continued through till Sunday morning Oct 21st, 2018 at 3:37 am when he finally let go. He was with family his final day and able to be fully present with his daughter and wife, two surviving siblings and his mother to say goodbye. We had a few tears, plenty of smiles and lots of talk about how grateful he was for the love and support all around him — family, friends, caregivers, and this extended community of you, his readers.
We will continue to maintain this site with more information and postings, albeit on a more limited basis. His last wish in his Will was to establish a fund for his daughter’s future education. Please follow this link to the GoFundMe site that we set up for the college fund.
https://www.gofundme.com/aubrey039s-education-fund
In the process of fulfilling Jeff’s wishes, like posting this announcement on his blog, I am frequently overcome by the love and support Jeff received from you, his readers, as well as from friends and family across the US. He loved well and was well loved.
Best,
Christopher Poehlmann
10-29-2018